While there are many different forms of vasculitis, all share the feature of organ damage caused by the immune system. Therefore, treatments for vasculitis are medications that suppress parts of the immune system (immunosuppressant drugs). The earliest treatment strategies developed for vasculitis involved very broadly-acting immunosuppressive drugs that lower immune system function in a relatively non-specific way. Today, vasculitis patients benefit from more sophisticated modern therapies that target specific portions of the immune system.
General Principles
We use a variety of medications, sometimes in combinations, to treat different forms of vasculitis. Yet a similar general approach is used across these diseases. Active vasculitis causes damage to the organs affected by the disease. We act quickly to stop the inflammation that is present in active disease. When successful, a patient then enters a state of disease remission. During remission, all signs of active inflammation are gone, but there may still be symptoms due to damage in organs where inflammation was previously present.
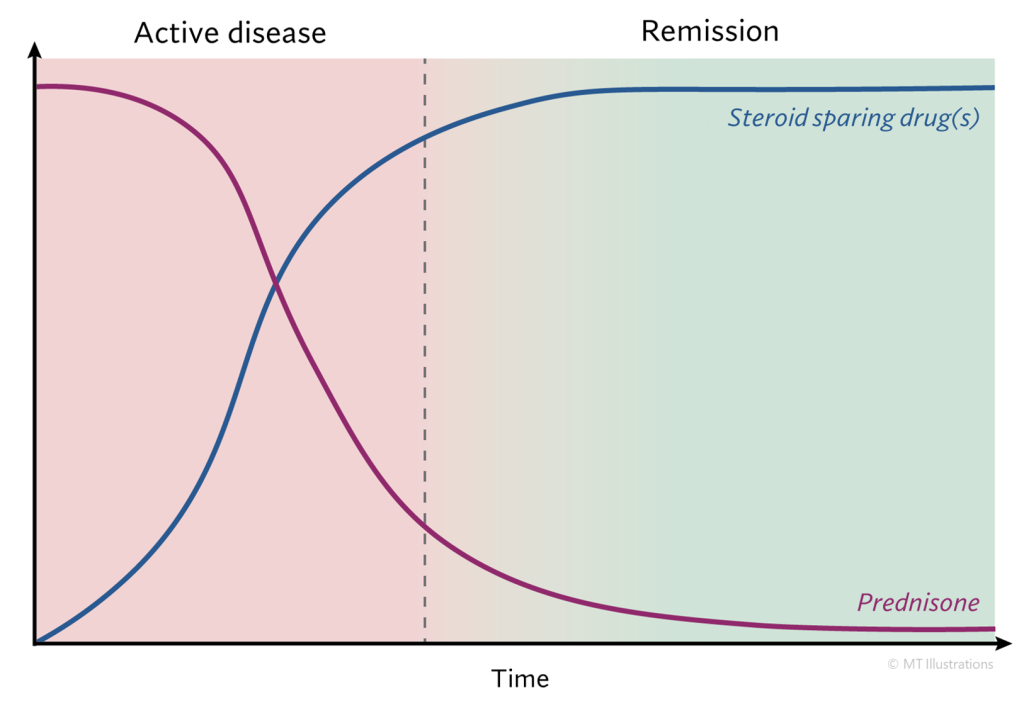
When disease is in an active state we typically use steroids (prednisone) to bring the disease under control quickly. The amount and type of steroids used depends on the severity of the inflammation present. Generally, steroids are used on a short-term basis to bring the disease under initial control (remission). We avoid long-term use of steroids because of their numerous and serious side effects. Some mild forms of vasculitis do not require any prednisone at all.
Along with the initiation of steroids, we typically start a “steroid-sparing” drug that will be used on a longer-term basis. These steroid-sparing drugs provide the antiinflammatory effect that controls vasculitis, while avoiding the side effects of steroids. Some steroid-sparing drugs are “biologic” medications – drugs that are made from cells, rather than chemicals synthesized in a reaction or extracted from a natural source. Examples of biologic treatments include insulin, vaccines, and blood products. In rheumatology, many biologics are antibodies that have been designed to target specific parts of the immune system. These drugs provide greater specificity than older drugs, therefore helping to reduce side effects. In addition to immunosuppressive drugs, we use some other treatments that are immunomodulatory in function – they have an impact on the immune system, but do not lower immune function in such a way that the risk of infection is increased. Examples of immunomodulatory drugs include colchicine and IVIG.
The first step in treating active vasculitis is to bring the disease into a state of remission. Prednisone impacts the immune system very quickly, and does the bulk of the work to reduce inflammation acutely. Most steroid-sparing drugs take longer to have an effect. After active disease has been adequately treated, our next goal is to reduce and then eliminate steroids, and use the steroid-sparing drug alone to maintain disease remission. Sometimes we are able to switch to milder immunosuppressants to maintain disease remission for longer timeframes. Occasionally, we are forced to maintain the use of prednisone for a longer time, but we always work to minimize the amount of prednisone used in these cases.
Once patients are successfully into remission, we continue using maintenance immunosuppression to keep the disease in a quiet state. The overall duration of therapy depends on many factors, including: the specific type of vasculitis present and its propensity to relapse, the severity and type of organ damage that was present at onset, the extent to which patients tolerate immunosuppression, other medical diagnoses that may be present, and other factors. Most forms of vasculitis have the ability to return to an active state at some point in the future, which is referred to as a relapse or flare of disease. In general, the symptoms that occur during relapses are less severe than those that were present at the beginning of a patient’s illness before immunosuppression had been initiated.
Below you will find information on the specific drugs that we utilize in the management of vasculitis.
Vasculitis medications:
- Prednisone
- Avacopan
- Apremilast
- Azathioprine
- Colchicine
- Cyclophosphamide
- Dapsone
- Intravenous or Subcutaneous Immunoglobulin (IVIG/SCIG)
- Leflunomide
- Mepolizumab
- Methotrexate
- Mycophenolate
- Rituximab
- Sarilumab
- TNF inhibitors
- Tocilizumab
All information contained within the Johns Hopkins Vasculitis Center website is intended for educational purposes only. Visitors are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website.