The term “vasculitis” refers to a group of inflammatory diseases that cause inflammation centered in the wall of blood vessels. This vascular inflammation ultimately leads to damage and dysfunction of the organs that contain the affected vessels. The symptoms of vasculitis depend on the particular blood vessels (and organs) that are involved by the inflammatory process.
As a group, the vasculitis syndromes have the ability to affect nearly every organ in the body. Yet different forms of vasculitis tend to involve blood vessels in specific locations throughout the body. For example, Giant Cell Arteritis typically involves the medium– to large–sized blood vessels supplying the head and neck, but rarely involves the blood vessels of the kidneys. In contrast, Granulomatosis with Polyangiitis (GPA) frequently involves the kidneys, very often the lungs, and almost always the upper respiratory tract, but rarely blood vessels to the brain.

As depicted in the image, Buerger’s disease involves the fingers (and toes). Gangrene can result from a profound lack of blood flow to these affected tissues.
Different types of vasculitis have characteristic (localized) patterns of blood vessel involvement. However, vasculitis is often a systemic illness. Thus, patients with vasculitis generally feel sick. They often have fevers, weight loss, fatigue, a rapid pulse, and diffuse aches and pains that are difficult to pinpoint. It has been said that vasculitis is a “hurting disease”, because it is so commonly associated with pain of one type or another: pain from a nerve infarction, pain from insufficient blood to the gastrointestinal tract, pain from skin ulcers. In some cases, however, identifying the source and underlying cause of the pain is extremely challenging. Because vasculitis can involve virtually every organ system in the body, it often masquerades as other diseases, and may be a challenging diagnosis to make.
What organ systems may be affected?
It is important to note that not every organ system will be affected in every patient. The pattern of organ involvement (and symptoms) is unique to the individual, as well as the type of vasculitis (category).
Skin
A variety of rashes, the most classic of which is “palpable purpura” –purplish–red spots, usually found on the legs. These spots can usually be felt by the examiner’s fingertips, hence the descriptor “palpable”.

This is a classic example of palpable purpura. These lesions result from the leakage of blood into the skin through inflamed, damaged blood vessels. They tend to occur in “crops”. This type of vasculitis involves very small diameter blood vessels in the skin.

Repeated bouts of purpura may lead to hyperpigmented (darkened) areas of the skin.
Joints
Symptoms range from full–blown arthritis to aches in the joints without obvious swelling (arthralgias).

This is an example of Henoch-Schönlein purpura: cutaneous vasculitis manifested by palpable purpura and arthritis (note the right ankle swelling). The diagnosis was confirmed by a skin biopsy, with immunofluorescence positive for IgA deposition witin blood vessel walls.
Lungs
Cough (particularly coughing up blood), shortness of breath, a pneumonia–like appearance to a patient’s chest X–ray, lung “infiltrates”, and the development of cavities in the lungs are among the manifestations that may occur in forms of vasculitis with lung involvement.
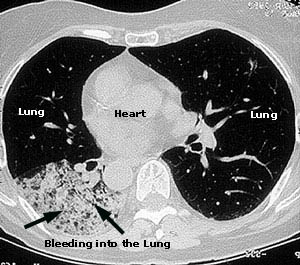
This image comes from a CAT scan of the lungs of a 73 year–old woman complaining of constitutional symptoms, shortness of breath, and bloody sputum. The patient also had glomerulonephritis (kidney inflammation), a positive P–ANCA antibody test, and antibodies to myeloperoxidase. The diagnosis of microscopic polyangiitis was made.
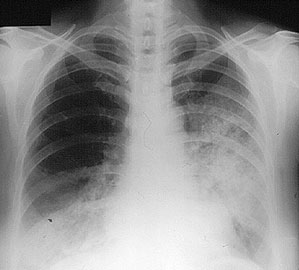
Eleven days later, as the patient’s symptoms worsened, a chest X–ray confirmed progression of her lung hemorrhage. The X–ray shows fluffy infiltrates in both lungs, representing bleeding from damaged capillaries.
Kidneys
In contrast to many other organs, inflammation in the kidneys does not hurt or cause other symptoms a patient would notice until renal damage is quite advanced. Instead, evidence of vasculitis involving the kidneys is made by obtaining lab tests, and in many cases a kidney biopsy. Glomerulonephritis is the most common type of kidney damage encountered in vasculitis. This syndrome can cause abnormal lab findings in the urine, including the presence of red blood cells (usually invisible to the naked eye), clumps of red blood cells (known as “casts”, also invisible to the naked eye), and abnormal levels of protein in the urine. If renal involvement is not recognized, renal failure can develop, sometimes leading to the need for dialysis or kidney transplant.
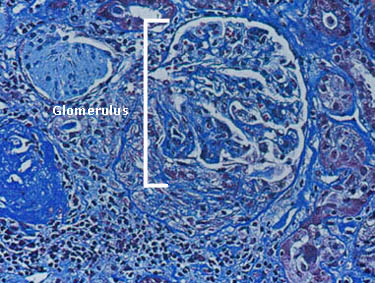
Depicted in the figure to the right is a single glomerulus (the filtering unit of the kidneys; each kidney has approximately 1 million glomeruli) as seen on a kidney biopsy. The glomerulus is the part of the kidney that is affected by small vessel vasculitis, such as ANCA associated vasculitis.
Polyarteritis nodosa (PAN) is another form of vasculitis that can involve the kidneys. PAN involves larger arteries that supply blood to the kidneys, and can be diagnosed using an angiogram (shown at right).
Blood
Vasculitis can cause abnormal findings on blood counts. Anemia (low hematocrit or red blood cell count) is a typical finding in patients with active vasculitis. A slightly elevated white blood cell count may also occur. These findings are very non-specific, meaning that they can occur in many other situations and diseases. Elevated inflammatory markers (erythrocyte sedimentation rate and C-reactive protein) are also frequently identified in patients with active vasculitis.
Sinus, Nose & Ears
The sinuses, nose and ears are common sites of involvement by ANCA-associated vasculitis, including GPA, EGPA and MPA. Symptoms can include chronic sinus congestion and “infections” that persist for longer than they should and require repeated courses of antibiotics; bleeding from the nose; perforations (holes) in the nasal septum; hearing loss; inflammatory fluid in the ears requiring drainage; inflammation in the cartilage of the ears or nose.

GPA involvement in the nose can lead to collapse of the nasal bridge (“saddle nose deformity”), as shown in the picture to the right.
Eyes

Vasculitis involving the eye may affect either blood vessels to the eyes, causing the sudden loss of vision, or small blood vessels within the eyes, leading to retinal problems, thinning of the sclera (the white part of the eyes), inflammation within the eye’s different chambers, and conjunctivitis (“pinkeye”). Pictured at right is an example of retinal vasculitis in a patient with systemic lupus erythematosus (lupus). The white areas represent regions of retinal infarction caused by vasculitis. The most feared complication of GCA is blindness caused by injury to the optic nerve.
Brain
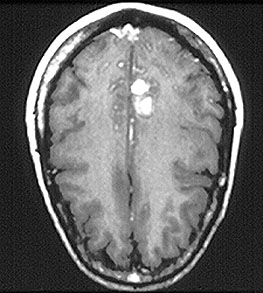
The brain is not a common site of vasculitis involvement. When present, vasculitis in this site can cause headaches, strokes, changes in mental status, or difficulty with coordination. At right, a magnetic resonance (MR) imaging study of the brain in central nervous system vasculitis demonstrates an intra–cerebral hemorrhage (bright area).
Nerve
Peripheral nerves are a relatively common site of vasculitis involvement. Damage to the peripheral nerves can cause shooting pains in the arms and legs, numbness, and asymmetrical weakness (i.e., weakness that involves one side of the body more than the other).
All information contained within the Johns Hopkins Vasculitis Center website is intended for educational purposes only. Visitors are encouraged to consult other sources and confirm the information contained within this site. Consumers should never disregard medical advice or delay in seeking it because of something they may have read on this website.