- First Description
- Who gets EGPA (the “typical” patients)?
- Classic symptoms of EGPA
- What causes EGPA?
- How is EGPA diagnosed?
- Treatment and Course of EGPA
First Description
Eosinophilic granulomatosis with polyangiitis (EGP), formerly known as the Churg-Strauss Syndrome , is a systemic vasculitis. This disease was first described in 1951 by Dr. Jacob Churg and Dr. Lotte Strauss as a syndrome consisting of “asthma, eosinophilia [an excessive number of eosinophils in the blood], fever, and accompanying vasculitis of various organ systems”. EGPA shares many of the clinical and pathological features of polyarteritis nodosa (“PAN”, another type of vasculitis) and granulomatosis with polyangiitis (GPA). However, Drs. Churg and Strauss discovered that the presence of granulomas as well as the abundance of eosinophils distinguished this disease from PAN and GPA.
Who gets EGPA (the “typical” patient)?
The typical patient with EGPA is a middle aged individual with a history of new-onset or newly-worsened asthma. The distribution of the disease among males and females is approximately equal.
Classic symptoms and signs of EGPA
Asthma is one of the cardinal features of EGPA. Asthma symptoms may begin long before the onset of vasculitis – e.g., many years before any other symptoms of EGPA arise, and long before the diagnosis of EGPA is made. Other early symptoms/signs include nasal polyps and allergic rhinitis.
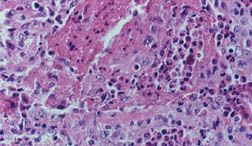
The next phase of the disease is often marked by eosinophilia, the finding of an excessive number of eosinophils in the blood or in tissues. An eosinophil is one subtypes of white blood cell. Normally, eosinophils comprise 5% or less of the total white blood cell count. In EGPA, the percentage of eosinophils may reach as high as 60%. In the picture below, the eosinophils are shown by the dark pink stain.
The third phase of the illness is a vasculitis, which involves the skin, lungs, nerves, kidneys, and other organs. Particular mention should be made of the frequent devastating involvement of the nerves (called mononeuritis multiplex), which produces severe tingling, numbess, shooting pains, and severe muscle wasting/power loss in the hands or feet. The list below contains the organs commonly involved by EGPA and the specific disease manifestation(s) in each organ.
Nose
- Sinusitis, including allergic rhinitis
- Nasal polyps
Lung
- Pulmonary infiltrates (only one-third of all patients)
- Bleeding into the lungs (occasionally)
- Diffuse interstitial lung disease (rarely)
Skin
- Rashes
- Palpable purpura
- Nodules (above or below the skin), often at sites of pressure, such as the elbows
Kidney
- Glomerulonephritis (inflammation in the small units of the kidney that filter blood)
- Hypertension
Gastrointestinal
- Lesions (vasculitic) are occasionally found in the GI tract
- Granuloma sometimes found in spleen
Heart
- Vasculitis lesions in heart, can lead to congestive heart failure or a heart attack
Nerve
- Peripheral nerve involvement including pain, numbness, or tingling in extremities (neuropathy/mononeuritis multiplex)
What causes EGPA?
The cause of EGPA is unknown but is probably multi-factorial. Genetics may play a small role in the disease, but EGPA is almost never seen in two members of the same family. Environmental factors such as exposure to industrial solvents may play a role in susceptibility to this disease, but this is largely speculative. Infections may be the inciting event(s), but to date there is no definitive evidence of this.
How is EGPA Diagnosed?
Among all of the vasculitides, asthma is a distinctive feature of EGPA alone. However, not all patients with asthma have vasculitis – only a tiny minority do, in fact. It is the specific combination of symptoms and signs, the pattern of organ involvement, and the presence of certain abnormal blood tests (eosinophilia, in particular) that help the doctor make the diagnosis. In addition to a detailed history and physical examination, blood tests, chest X-rays and other types of imaging studies, nerve conduction tests, and tissue biopsies (e.g., of lung, skin, or nerve) may be performed to help diagnose EGPA.
The following features are consistent with a diagnosis of GPA:
- asthma
- eosinophilia [>10% on differential WBC count]
- mononeuropathy
- transient pulmonary infiltrates on chest X-rays
- paranasal sinus abnormalities
- biopsy containing a blood vessel with extravascular eosinophils.
Treatment and Course of EGPA
EGPA usually responds to prednisone. Initially, high doses of oral prednisone are used in an attempt to get the disease into remission as quickly as possibly (e.g., using oral prednisone 40-60 mg/day). After the first month or so, this high dose of prednisone is gradually tapered down over the ensuing months. Other immunosuppressive drugs, such as azathioprine, cellcept, methotrexate, cyclophosphamide, or rituximab may be used in addition to prednisone. High doses of intravenous steroids (usually methylprednisolone) maybe useful for those patients with severe disease or for those who are unresponsive to the combination of oral prednisone used with other immunosuppressive medications.
Prior to the advent of prednisone, EGPA was often a fatal disease. The majority of patients died from rampant, uncontrolled disease. With present therapy, constitutional symptoms begin to resolve quite quickly, with gradual improvement in cardiac and renal function, as well as improvement in the pain that results from peripheral nerve involvement. The course of therapy can last for 1 to 2 years, although the length and type of treatment depend on the severity of disease and the organs involved. The patient’s response to treatment and the continuation of disease control during lowering of the prednisone dose are the primary determinants of how long therapy is continued. Laboratory monitoring of blood tests is very helpful in gauging the activity of disease. Some of the most useful laboratory tests are the erythrocyte sedimentation rate (ESR) and the eosinophil count.